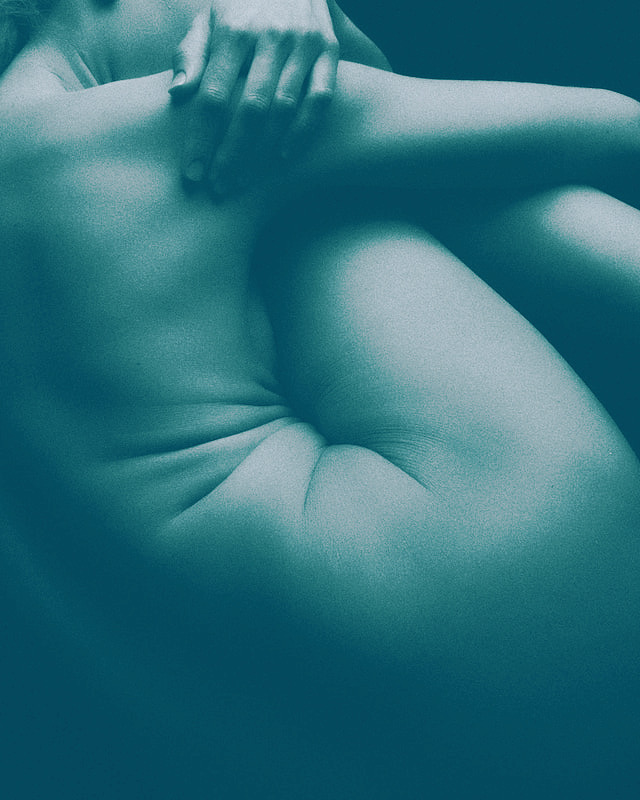
Endometriosis. What can be done?
There are a wide range of symptoms and each person’s symptoms are different to the next person. The major symptoms of endometriosis are:
- Pelvic pain. Pain can present as lower abdominal pain, vulval, anal pain. It can refer to other areas around the pelvis such as the lower back and hips. In some women her pain can refer down the legs or sometimes up into the chest
- Pain can occur with vaginal penetration such as with intercourse and using tampons, pain with bladder and/or bowel function
- Ovulation pain
- Painful and/or heavy periods and abdominal cramping
- Abdominal bloating
- Urinary frequency and/or urgency
- Bowel changes either constipation or diarrhea. It can sometimes be mistaken for IBS
- Fatigue and mood changes are also quite prevalent
- Infertility
Unfortunately, a diagnosis still requires a laparoscopic procedure and biopsy to confirm endometriosis. Surgery removes the endometriosis, and in some cases, it helps with one’s pain. However, there are some women where pain still persists after surgery. It’s not that surgery was a failure, but sometimes there are other underlying factors contributing to pain. So does this mean that you need to have another surgery soon? Health professionals are aware that with each surgery you have, this increases scar tissue and adhesions developing, which can also play a role with pain. We definitely do not want to increase your pain!
As a pelvic floor physiotherapist, we can play a role in assessment and management of pain. The pelvic floor is likely to develop tension as a consequence to try to manage the pelvic pain and any other associated symptoms. So what is one of the main key things we are hoping your pelvic floor to do? It’s to teach it how to relax. So for example if you ball your hand into a fist and it stays that way 24/7 it’s going to hurt at some point. So imagine that being your pelvic floor.
Other treatments may include stretches and tailored exercise ideas, encouragement of relaxation through positioning, general advice on meditation, usage of vaginal trainers and optimising bladder and bowel habits. Some women may not get the desired result, some get significant reductions in pain. Our goal though is not to cure endometriosis, as it is a chronic condition, but more so to manage the symptoms.
1. Endometriosis Australia, Endometriosis Australia, https://www.endometriosisaustralia.org/
Related Articles

Endometriosis. What can be done?
Pregnancy related pelvic pain and everything starts to get a little bit too much

Prolapse and Pessaries
Pregnancy related pelvic pain and everything starts to get a little bit too much

I have a prolapse, now what?
Pregnancy related pelvic pain and everything starts to get a little bit too much