
You have a prolapse, now what?
The dreaded word – prolapse. No woman ever wants to hear this word nor do I wish that any woman experiences it either. Unfortunately though it is a lot more common than what people think it is, but just not talked about.
So let’s start, what is a prolapse you ask? We have pelvic ligaments, connective tissue and fascia that are designed to hold our organs up in place. A prolapse is when the pelvic tissues stretch and the organs descend down into the vagina. A prolapse can happen suddenly or occurs gradually over time. But there are a few types of prolapse and sometimes regretfully some women can have multiple prolapses.
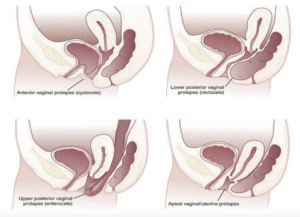
- Bladder prolapse (otherwise medically known as a cystocele)
- Bowel prolapse (rectocele)
- Uterine prolapse
- Vault prolapse – If you have had a hysterectomy, sometimes the top of your vaginal wall can still descend down
- Enterocele – rare, but sometimes your gut can descend down into the vaginal wall
The main symptoms of prolapse, which I am sure everyone has googled are:
- Vaginal bulging and/or heaviness
- Back pain
- There can be changes to your bladder or bowel function. And that can range from not being able to empty your bladder, stop start flow with voiding, urinary urgency, sometimes incontinence and constipation, requiring digitation to help empty bowels
So what causes a prolapse one might ask? That differs between each woman but it can be:
- Having been pregnant and having a vaginal birth (though isn’t limited to those that have had caesareans)
- Repetitive straining with daily activities or job descriptions or chronic coughing
- Constipation
- Being overweight
- Menopause
- Possibly genetic makeup of your tissues
- If you have had previous pelvic surgery
So once the ligaments and connective tissues have stretched, there are typically two options of treatment. The conservative or the surgical management. Let’s delve into the surgical part first.
So like any surgery, the goal is to get you into tip top shape before you have your surgery with the aim to optimise your recovery post op. Success rates of surgery will vary between individuals but things like age, weight and other co-morbidities and in this case, the genetic makeup of your tissues can determine the outcome.
I also reiterate to patients as well that having prolapse surgery carries the same risk as any other surgery with risk of infection, possible postoperative pain and the mandatory 6 week period of rest and no heavy lifting. So any woman at that stage in their life, if there are young children or spouses to look after this is something to take into strong consideration.
So if you have knee or hip replacement, the ideal scenario would be to try to get into shape and get as much strength into the knee or hip to help with the recovery. The same principle will apply to your pelvic floor too with prolapse surgery. So what are some of the easiest things to do?
- Maintaining a healthy body weight. Increasing weight puts more strain and pressure on your pelvic ligaments and tissues that can then lead to further stretching
- Get your bowels into top shape. If there is a history of constipation, we want to minimise the need to strain. So whether that be through diet/fibre, fluid intake, exercise or laxatives to help assist
- Speak to us about a pelvic floor exercise programme. Having an individual program is going to help get the right technique and frequency.
Then post operation is giving yourself the time to recover and slowly and gradually resume your pelvic floor exercises. Speak to your physiotherapist about returning to exercise safely particularly if you enjoy high intensity exercise and ensure the pelvic floor exercise programme is the right one for you.
Related Articles

Endometriosis. What can be done?
Pregnancy related pelvic pain and everything starts to get a little bit too much

Prolapse and Pessaries
Pregnancy related pelvic pain and everything starts to get a little bit too much

I have a prolapse, now what?
Pregnancy related pelvic pain and everything starts to get a little bit too much